-
Bladder Health
-
Prostate Health
-
Testicular Health
-
Urinary Health
-
-
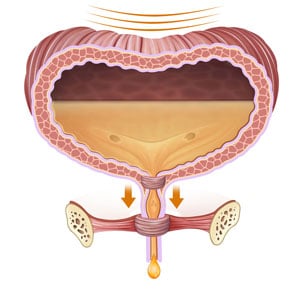
Bladder Health
-
Urinary Health
-
Vaginal Health
Specialized Care for Women’s Specialized Needs
TUCC doctors and advanced practice providers have vast expertise and experience caring for women.
Our physicians and surgeons focus only on urologic specialties, and we attract the very best in their fields.
-